Brief • 2 min Read

As the COVID pandemic continues, states have begun to lift stay-at-home restrictions. Fear continues, however, and people are still seeking to minimize unnecessary social contact. The Harris Poll is continuing its exploration of the state of telehealth in America, which has seen – a significant increase in use of telehealth during the pandemic.
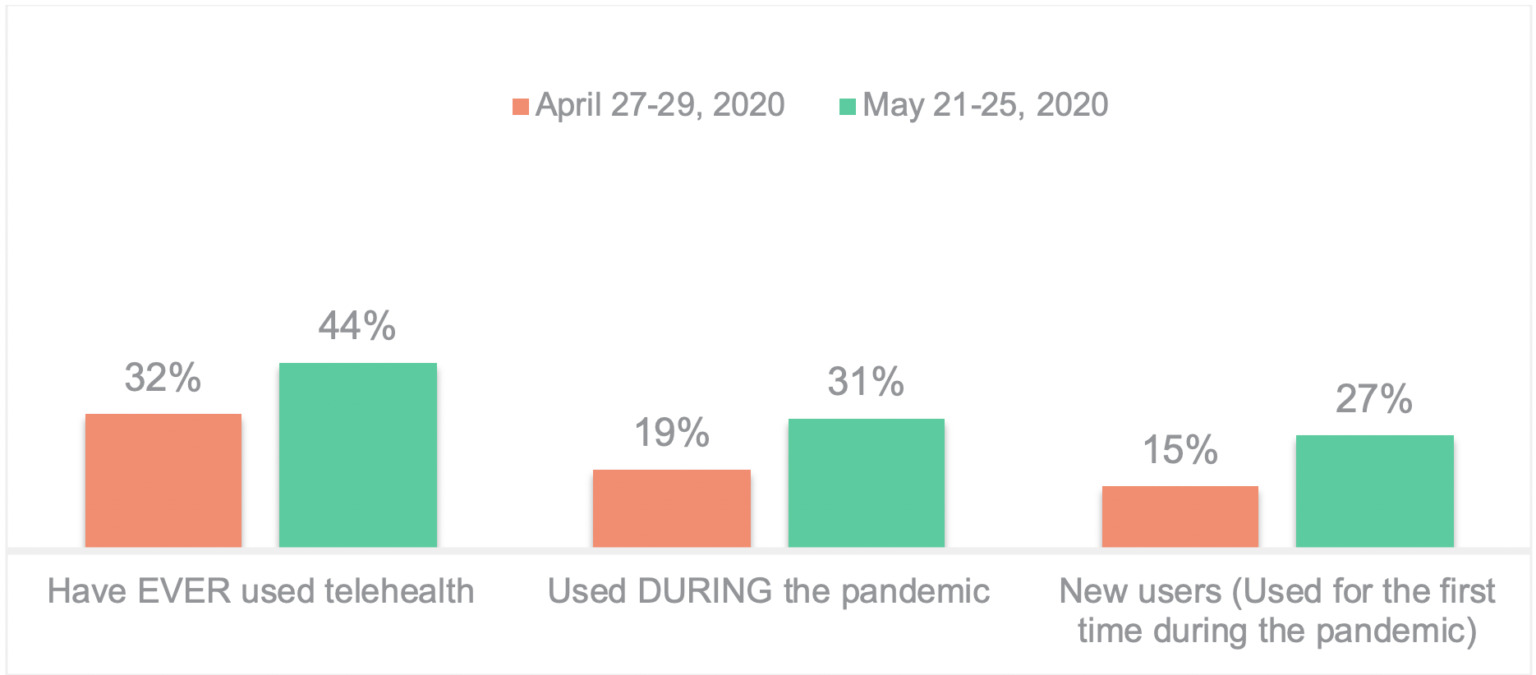
After the first six weeks of lockdown, (initial fielding, April 27-29, 2020), 32% of Americans had used telehealth services; less than a month later, (May 21-25, 2020) 44% have now ever used telehealth. Among Americans who have ever used telehealth, 70% used it during the pandemic. Since the end of April, “New users” of telehealth have increased from 15% to 27% of all Americans.
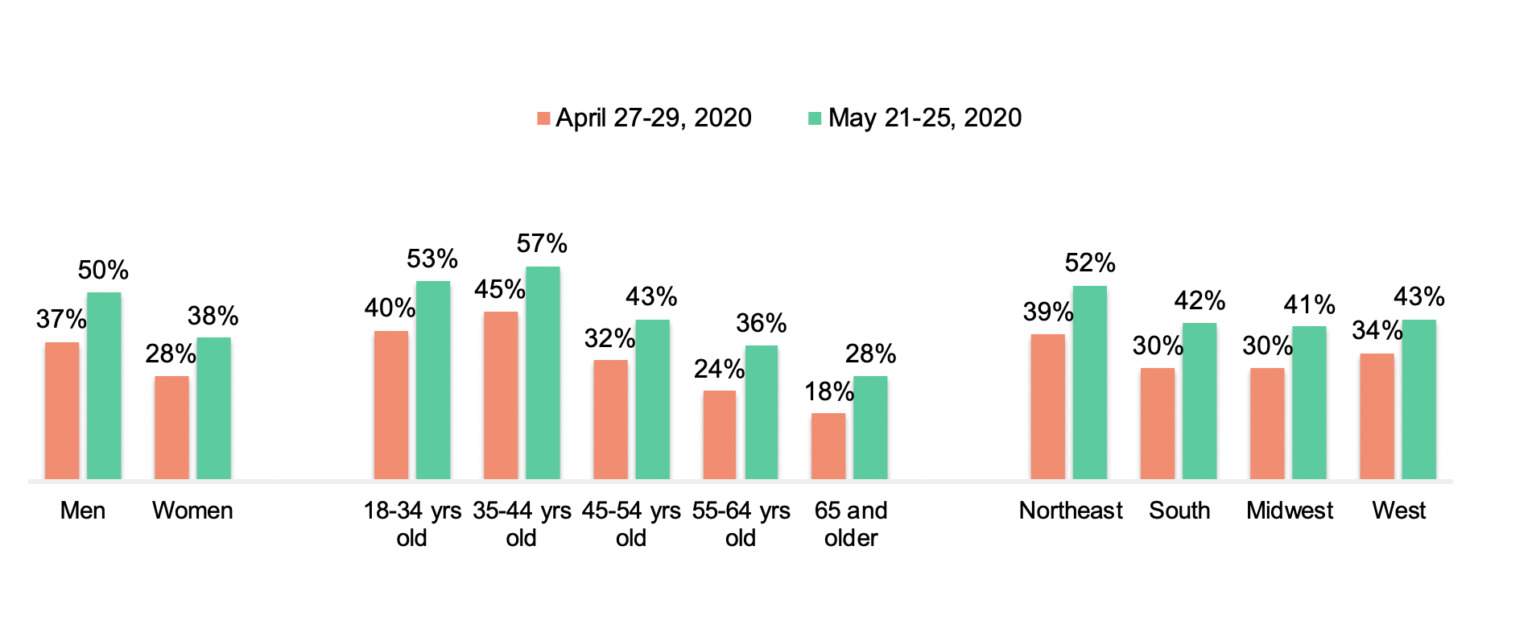
The uptick in telehealth usage over the last month is consistent across demographic groups. Usage is up among men (37% – 50%); younger adults are still more likely to have used telehealth than their older counterparts – but there is a notable increase in usage among Americans 65+ during this time frame (18% to 28%). Usage is more pronounced in the NE sector of the country (52% today versus 39% previously) (which has been more impacted by the pandemic), but over four in ten indicate usage in other regions (South, Midwest, West). Usage is distributed relatively evenly across ethnicity.
Frequency of use increased during COVID
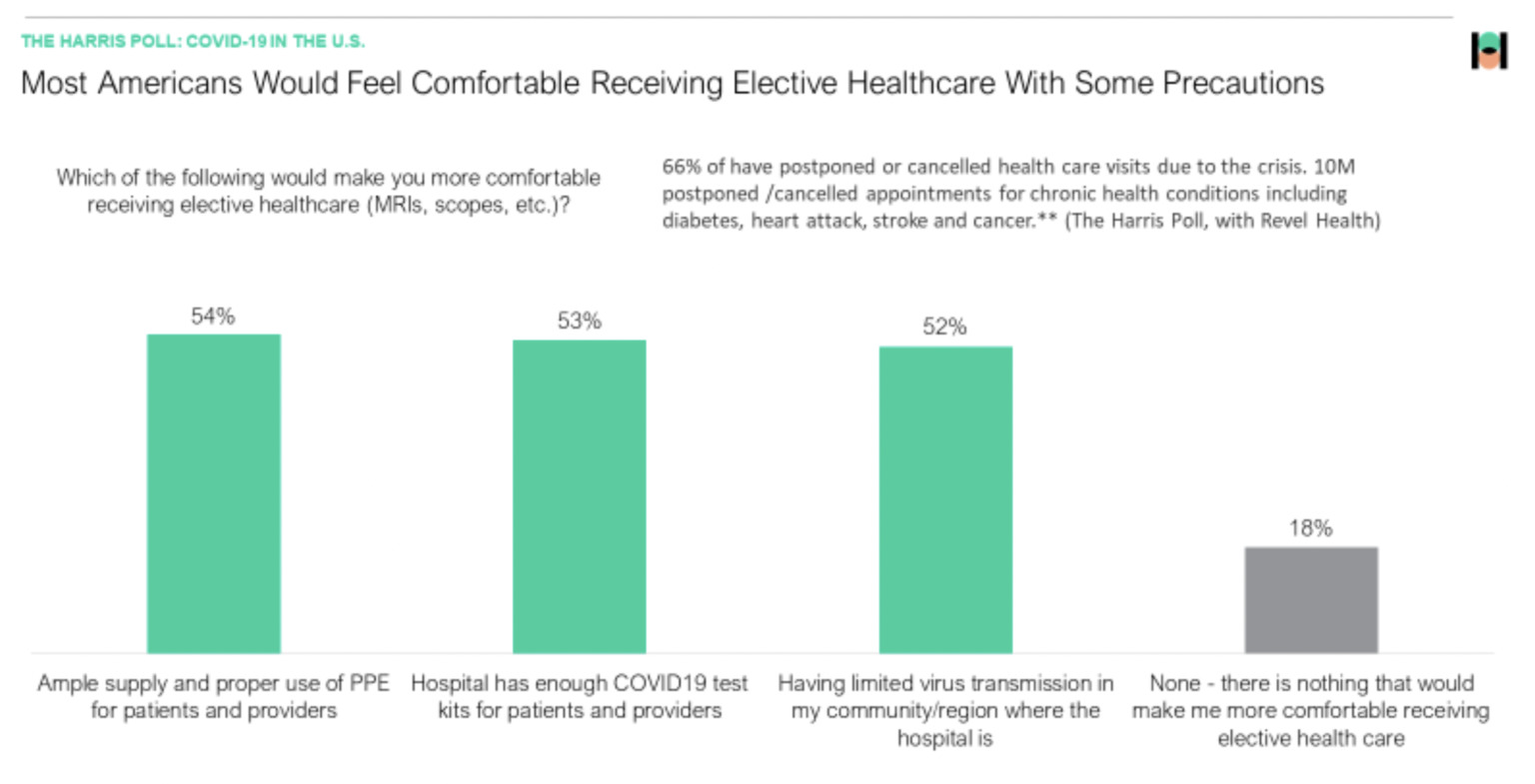
As revealed in the Harris Poll COVID tracker (Week of May 12, 2020) over half of Americans are still reluctant to engage in a traditional health care setting (for non-emergency visits) unless specific conditions were met. Nearly two in ten (18%) indicate that they wouldn’t be willing to go to a doctor’s office for elective healthcare under any circumstances.
As such, it’s no surprise that telehealth utilization rates are increasing not only overall, but also in frequency of use. During this compressed 3-month time frame since the pandemic began, nearly four in ten (37%) have used telehealth services three or more times.
Overall, among those who use telehealth services, more than three-quarters are using telehealth services for themselves, while two in ten are doing so on behalf of a child or on behalf of their spouse/partner.
Usage for Management of Chronic Conditions Increases During Pandemic
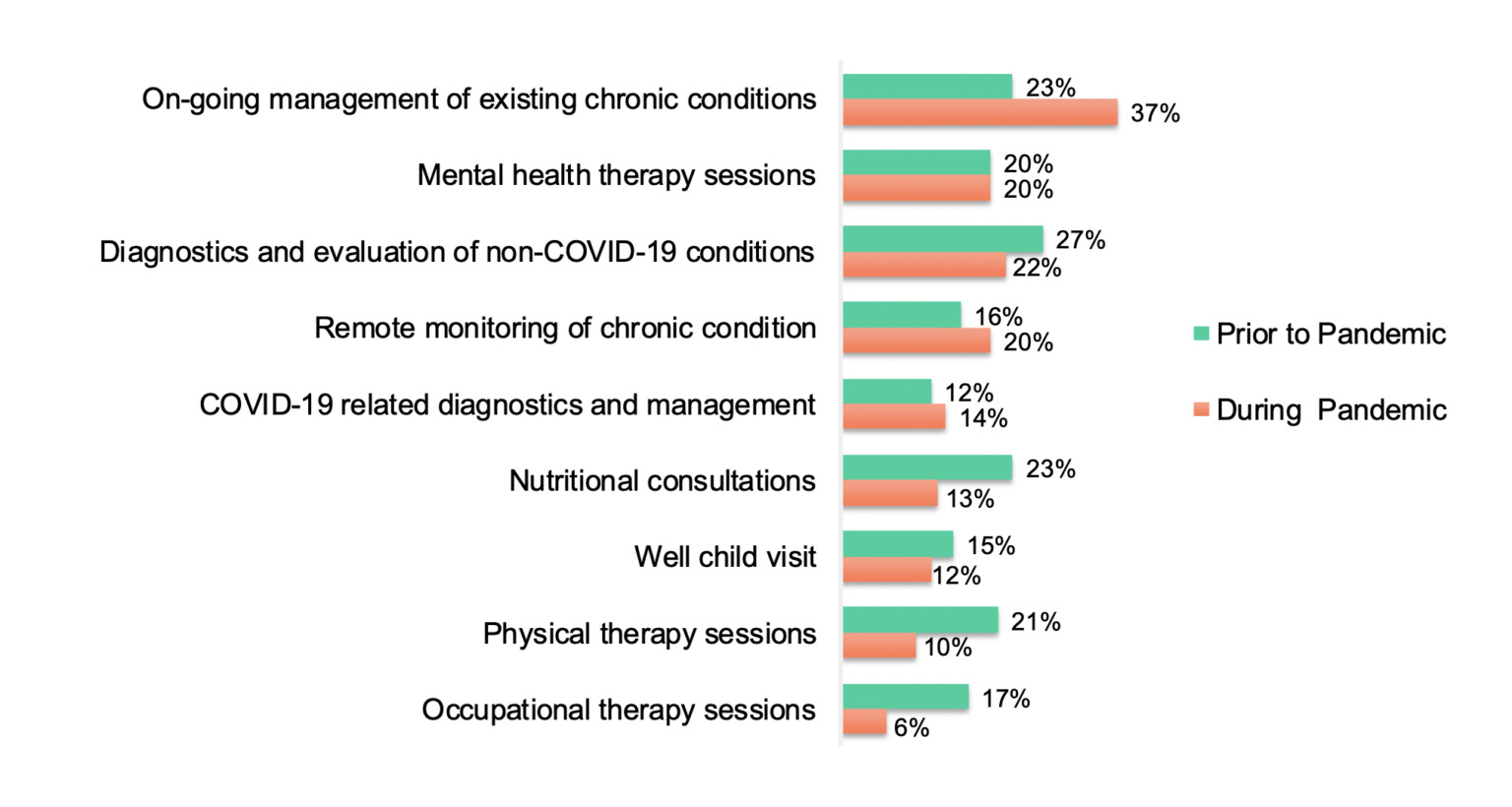
There is often a tendency to think of telehealth services as a convenient solution for seeking medical care or advice when there is an urgent need, but the pandemic has highlighted telehealth as a means of monitoring chronic conditions.
Overall, telehealth continues to be used for a diverse set of applications including mental health services, diagnostic visits (for non-COVID and COVID-related conditions), nutritional consultations and physical/occupational therapy sessions.
There has been an increase in ongoing management of existing chronic conditions and remote monitoring of chronic health, as well as a particularly notable uptick among those in the 65+ age group for using telehealth for ongoing management. (Wave 1: 58% versus 64% in wave 2).
Health care – and our comfort with technology
Technology is playing an important role in pandemic communications in general, and telehealth is no exception. In this round of research nearly two-thirds of (64%) say they accessed telehealth using a camera of some type – whether on a smartphone (41%) or a computer-based camera (36%). Nearly nine in ten telehealth users (86%) expressed satisfaction with the technology aspect of their telehealth experience. Other Harris Poll research indicates that 39% of Americans 65+ say they use video calling and 17% reported increased usage during the pandemic. Only 5% said they experienced any challenges.
The question for the future turns on whether the “relaxed” HIPAA guidelines for using more consumer based platforms (e.g., Facetime, Zoom)* will remain in place once the pandemic subsides. This flexibility, along with the loosening of other guidelines regarding physician licensure, etc., may be pivotal as to whether telehealth persists as a go-to application.
Telehealth “delights” on a variety of parameters
In our initial telehealth research (at the end of April), 82% of those who had used telehealth said they “liked it” or “loved it”. This time around we dug into some of the factors that combine to support that positive perspective.
At a high level, most individual aspects of the telehealth experience contribute to a high level of satisfaction. Overall “ease” of accessing needed health services, including prescriptions, is key, and nearly nine in ten indicate strong satisfaction with ease of getting prescriptions, securing an appointment, and accessing follow-up care. The same percentage indicates that they feel very comfortable with the confidentiality of their interaction with their healthcare provider during the appointment.
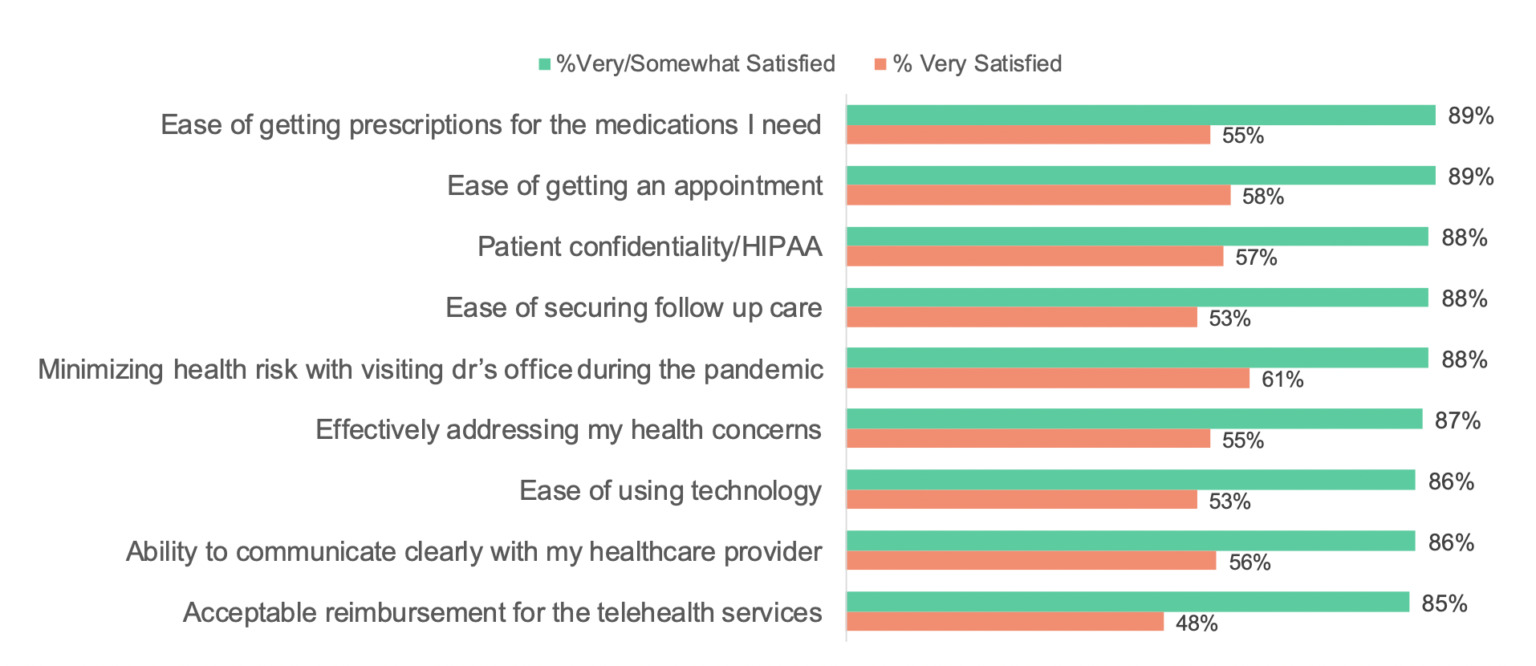
Future use of telehealth remains promising
As in our initial wave, nearly eight in ten (79%) of those who have used telehealth indicate that they are likely to continue doing so after the pandemic subsides; 40% of users say “very likely”. While the data is positive across many aspects of telehealth services, we should note that there is one variable that emerges as a key driver of Americans’ willingness to keep using telehealth services – and that is that it’s simply effective. When examining the data via regression analysis, the fact that telehealth is able to ‘effectively address my healthconcerns’ carries twice the impact of most of the other items evaluated.
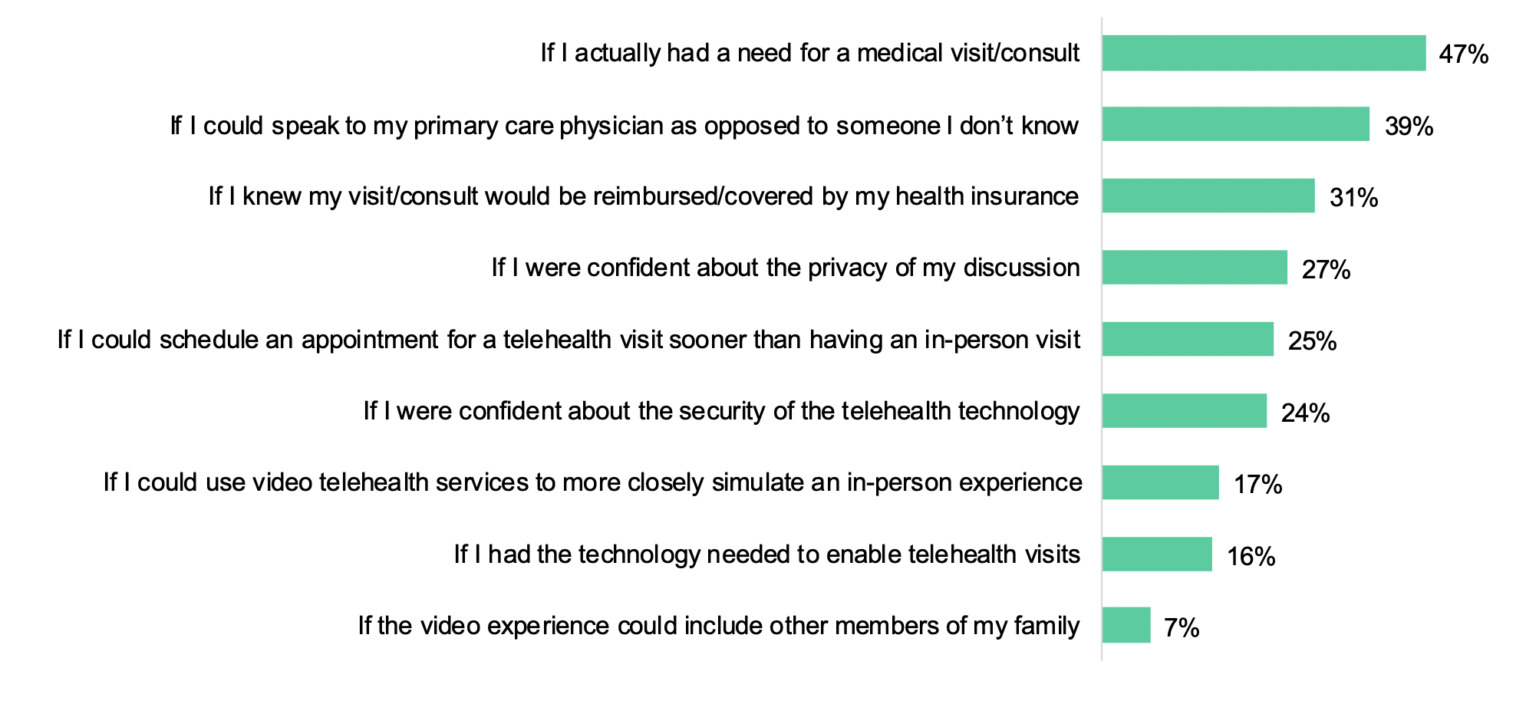
The patient-physician bond is critical in encouraging usage
Besides the obvious criteria for needing health care at all, four in ten (39%) of non-users say that they would be more willing to use telehealth if they could be assured of speaking to their own physician as opposed to someone they don’t know. This sentiment is most prevalent among seniors 65+ (cited by 52%) along with needing reassurance of reimbursement (40%).
The elephant in the room: Reimbursement
Previous data provided by the Kaiser Family Foundation indicated that ~49% of the US population had insurance through employer sponsored plans. However, KFF indicates that “between March 1, 2020 – May 2, 2020 we estimate that nearly 78 million people lived in a family in which someone lost a job. Most people in these families (61%) were covered by ESI prior to job loss.” ** This data aligns with the current sample which indicates that 39% of Americans surveyed were covered by employer sponsored plans. Due to the continued fluctuations in the job market this figure is not likely to stabilize for some time.
Changes to Medicare in 2019 opened the door for broader of use of telehealth, extending coverage to virtual check-ins and e-visits and eliminating the requirement that users live in a rural area. At the outset of the pandemic, the US Department of Health and Human Services (HHS) approved broader use of telehealth services as part of the Coronavirus Preparedness and Response Supplemental Appropriations Act, providing for reimbursement of telehealth services at the same rate as in-person medical services. In April 2020, additional changes allowed for provision of psychology services by phone without video interaction. However, future policies regarding technology and reimbursement remain to be seen, particularly among employer-based plans.
*Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID19 Nationwide Public Health Emergency, March 30, 2020
** Eligibility for ACA Health Coverage following job loss”, Kaiser Family Foundation. May 13, 2020
Subscribe for more Insights
Subscribe to our newsletter for the latest trends in business, politics, culture, and more.
Related Content